Talk to your healthcare provider if you have type 1 or 2 diabetes and are considering starting a family. When it comes to reducing the chance of pregnancy difficulties and the loss of a baby, several things should be done before conception.
How vital is it for me to plan my pregnancy?
A woman who has type 1 or type 2 diabetes should take special precautions before getting pregnant and during her pregnancy. Type 1 or type 2 diabetes increases your risk for both the baby and yourself during pregnancy. Although you can’t eliminate all of these hazards, there are numerous things you can do to minimize them.

A diabetic woman’s guide on getting ready for a pregnancy
Talk to your doctor or diabetic team first. Specialists in pre-conception care may be sent your way.
Pregnant women with diabetes and pregnant women with diabetes should be aware of how each affects the other. You’ll also be provided information about local resources available to you during your pregnancy, including phone numbers for medical emergencies.
Infertility should not be negatively impacted by diabetes (your ability to get pregnant). Talk to your doctor if you have reproductive problems.
The greatest way to ensure a safe pregnancy is by following a few simple precautions before you get pregnant.
Make sure your HbA1C level is at the optimal level.
For the past two to three months, your HbA1C indicates your average blood glucose level. The smaller the chance of miscarriage, birth abnormalities, or stillbirth, the closer it is to your optimal level. In most cases, a blood glucose level under 48 millimoles per liter (mmol/L) will be diagnosed by your medical staff (6.5 percent).
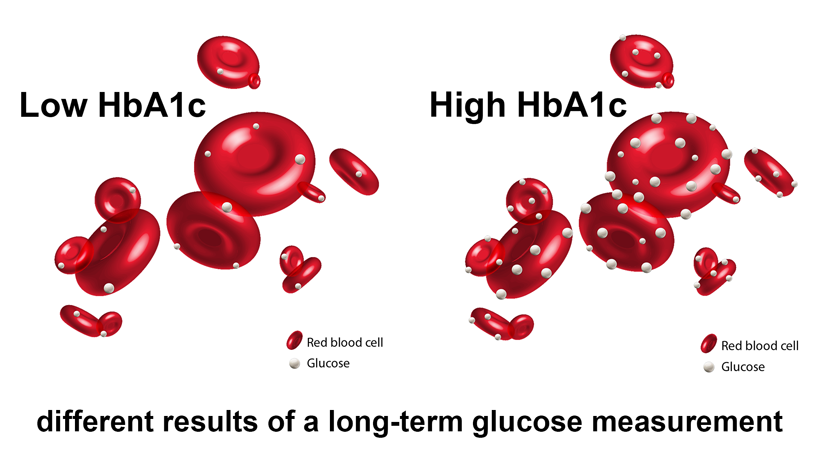
If your blood sugar levels are excessively high, your healthcare team will urge you to control them more closely before getting pregnant. HbA1C levels will be checked every month until they reach the prescribed values.
Keep using contraception and prevent pregnancy until you can lower your HbA1C levels to a safe level (above 86mmol/mol or 10 percent). There is a lower chance of miscarriage, abnormal births, and infant death as a result of this procedure.
Take a blood sugar reading.
Preventing gestational diabetes is essential since the first eight weeks of pregnancy are critical for the growth and development of your unborn child. First-trimester pregnancies might be difficult to detect. As a result, it is recommended that you utilize contraception until your blood glucose levels are ready for pregnancy. It’s better to prepare your glucose levels 2-3 months in advance of stopping contraception because you won’t know whether you’re pregnant right away.
When you’re getting ready to establish a family, you’ll need to pay extra attention to your blood sugar. Checking your blood glucose more frequently than usual will help you better understand how diabetes affects you and how you can manage it. Tests before and after meals are included in this. To keep your blood sugar levels in check throughout pregnancy, you’ll be advised by your healthcare team.
Increase your folic acid intake.
Taking folic acid can help prevent spina bifida in women who are hoping to get pregnant. Diabetic women should take a larger dose of folic acid since they are more likely to give birth to children with these diseases (5mg per day). Because this greater dose is not accessible over the counter, it must be prescribed by a doctor.
Folic acid can lower the risk of birth abnormalities by more than 70 percent if taken at least two months before conception. The best thing to do is take folic acid 2 months before you stop taking contraception because you won’t know immediately whether you’re pregnant. If it’s taking you longer to conceive, talk to your doctor about your folic acid consumption.
For the first 12 weeks of pregnancy, you should continue taking folic acid.
Pregnancy without taking folic acid isn’t a problem. Many ladies have had healthy kids in this scenario.
Make sure you’re taking your medicine as prescribed.
Pregnant women should check with their medical team to see if any medicine for diabetes (including insulin) and its complications is safe to use. Pregnant women can safely use Metformin, but they must cease taking any other glucose-lowering medications.
Other recommended drugs, such as statins, should be discontinued as well.
If you are taking other injectable drugs for type 2 diabetes, such as Victoza (liraglutide) and Byetta (exenatide) or similar, you will need to consult your doctor. Pregnant women should avoid them.
Don’t stop taking a prescription medicine without consulting your doctor first.
During pregnancy, your body’s ability to utilize glucose may vary, thus your diabetes treatment may have to be adjusted. After using medications for Type 2 diabetes, you might switch to insulin injections. To help you regulate your blood sugar levels, insulin pump treatment may be a viable option if you are currently taking insulin injections. You’ll get further information from your diabetic team.

Check your kidneys and eyes for any problems.
You should get a general health check from your doctor or diabetes team, including a check of your eyes and kidneys. You may be sent to a specialist team for further evaluation if there are any concerns. This part of the body is already in danger because of the increased pressure of pregnancy. Therefore, your checks will be repeated throughout the pregnancy, generally once every three months.
Before you quit taking contraceptives, have a renal (kidney) evaluation and any therapy you may require.
Look at your lifestyle
You may take steps to enhance your overall health and prepare your body for pregnancy, such as exercising and eating right. Stopping smoking, improving your food, increasing your physical activity, and, if necessary, reducing your weight are all included in this plan.
Doctors and nurses should provide you with weight-loss counseling when you have a BMI of more than 27. To avoid harming yourself and your unborn child, you should not diet while you’re pregnant. You may, however, make sensible modifications to your food and lifestyle throughout pregnancy to keep your weight in check.
Check to see if you have the proper vaccinations.
Check to see whether you’ve received your rubella or MMR shot if you haven’t had rubella before now. Ask your doctor if you’re unsure if you’ve been vaccinated before. The fact that you have already had it doesn’t make a difference, and it will set your mind at ease.
MORE THINGS TO BE AWARE OF:
A means of conducting tests
A blood ketone meter and testing strips should be provided to those with Type 1 diabetes. If your blood glucose levels are abnormally high, or you become otherwise ill, you can use them to check for ketones. If your ketone levels are abnormally high, you should seek medical attention right away.
You may also check your blood glucose levels with a CGM or a Flash Glucose Monitor.
Metformin
Despite Metformin’s patient information leaflet’s recommendation that it should not be used during pregnancy or while pregnant, it is increasingly being utilized in women with gestational and type 2 diabetes. Many nations use Metformin to control diabetes during pregnancy and lactation.
Before making any changes to your blood sugar levels
A recent eye exam and any treatment is a must before making any drastic dietary or lifestyle changes before becoming pregnant. Pregnant women who keep their blood sugar levels under control have a lower chance of developing eye issues. Diabetic eye issues (retinopathy) might worsen if blood glucose control is improved too quickly. Consult your diabetic eye specialist if you’ve experienced major eye difficulties.

