Introduction
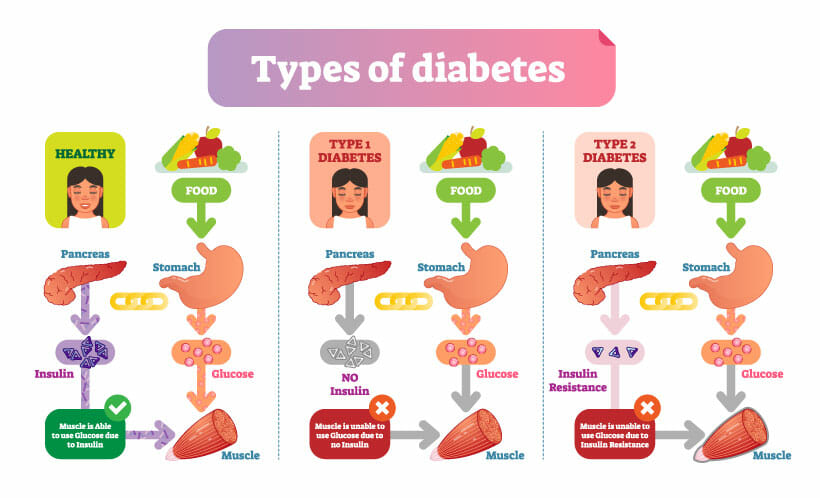
High blood sugar is a symptom of diabetes mellitus, a metabolic disorder that prevents the body from absorbing glucose from the blood into the cells. Insulin is responsible for transporting sugar from the bloodstream into the cells and consequently into the organs. It could be described as the key that lets the sugar into the cells. In the cells, the sugar (glucose) is stored or immediately used as fuel for the processes in the body. The most significant amount of glycogen in the body, up to 150 g, is stored in the liver. Our muscles keep up to 1% of their weight; this is enough for up to 90 seconds during intense exercise in sports or when we have to escape from a mountain lion.
In the German-speaking region of Europe, approximately 9 million people are currently affected by diabetes mellitus. In Germany alone, the costs of diabetes and its secondary diseases amount to 35 billion euros. Let’s look across the pond. In the United States of America, there are 34.2 million people of all ages—or one in ten. According to WHO/CDC and other diabetes institutions, one in five people (18 years and older) do not know they have diabetes. This represents about 3 percent of all adults. Diabetes becomes more common with age. Comparing international studies and statistics, it is noticeable that more than 26% of retirees aged 65 and over are affected by diabetes. The statistical ratios remain the same in industrialized countries, although there are upward and downward variations. The World Health Organization (WHO) is trying to draw attention to Diabetes Mellitus as diabetes numbers have increased massively in recent years. They expect 630 million diabetics worldwide in 2045, and one estimate in the 2019 IDF Diabetes Atlas is that there will be 700 million people. (IDF = International Diabetes Federation)
Diabetes is not a “modern” disease; on the contrary, it has been going on for countless generations. Archaeologists have found the first records on papyrus in Ancient Egypt, dated 1552 BC. It is not clear from it whether it is diabetes. When the mummy of Pharaoh Hatshepsut is examined, it turns out that she suffered from obesity, diabetes, and cancer. In 100 A.D., the Greek Aretaios used the word diabetes for the first time. At that time, ants proved the diagnosis, they love everything sweet, so they were all over it.

In ancient times, there were already the first medicines—licorice was very popular for treatment. In almost every century, there are corresponding records about the disease, but proper therapy has existed only since 1921. 1921, insulin was discovered by Mr. Banting and Mr. Best, which saved the lives of countless diabetics.
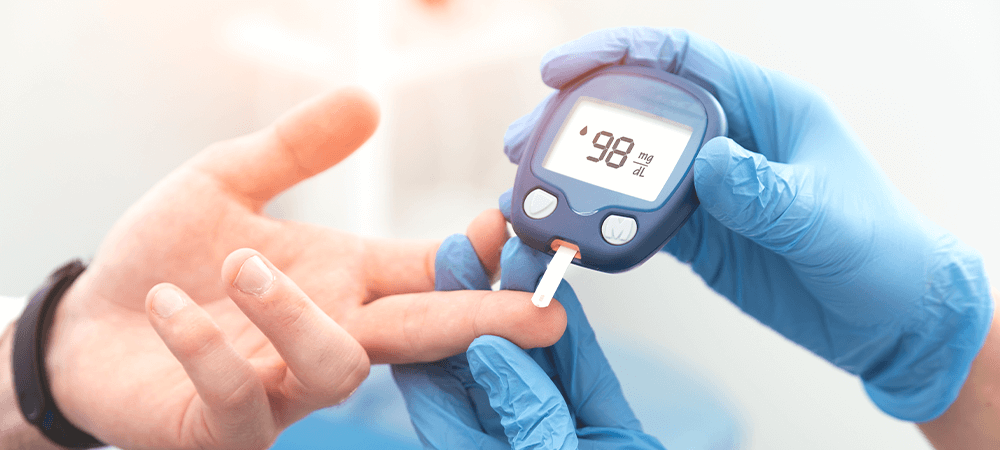
The next step was to provide ways to tailor diabetes therapy to individual needs, but this required blood glucose meters. In the 1980s, the first models appeared on the market, unsuitable for home use due to their size and price. Over time, the devices became smaller and also cheaper; today, we can already get them for under 50 euros. Meanwhile, there are other options, which are predominantly preferred by the mobile generation.
But what is diabetes mellitus in all its subgroups? Simply summarized, the body does not produce enough insulin, or its cells cannot use it because they are resistant to insulin. This causes blood glucose levels to be too high because glucose is no longer absorbed into the cells. The problem with this is that this sugars in the blood can become extremely dangerous for our organs, blood vessels, and nerves and damage them permanently.
In our advisors, you can find an overview of diabetes mellitus, the different types, symptoms, treatments, and possible preventive measures.
Diabetes – is divided into several types.
Diabetes mellitus is an umbrella term for one of the most common metabolic diseases in humans due to an elevated blood glucose level.
In the following sections, we explain the different types of diabetes and their variations.
Pre-diabetes
Diabetic pre-diabetes is also called early diabetes or diabetes precursor. The names are already clear that this is the first “stage” of diabetes. Although your blood glucose levels are already elevated, you do not need to be diagnosed with diabetes yet. This is because your blood glucose levels are above the norm but still below the defined levels (long-term glucose HbA1c > 6.5%) of diabetes.
Pre-diabetes can last for several years, which is why many people with diabetes do not even know they have diabetes yet. If you believe the statistics of the International Diabetes Foundation, we are talking about around 471 million people worldwide suffering from pre-diabetes in 2035.
People with elevated blood sugar levels (pre-diabetes) have a higher risk of developing diabetes mellitus, primarily type 2, than people with normal sugar levels.
How do you make a pre-diabetes diagnosis?
Monitoring blood glucose levels over a more extended period is essential for diagnosis. There are three possible tests, of which the long-term glucose HBA1C is the most informative, as it provides an overview over 2 to 3 months.
- Long-term sugar HbA1c in %: between 5.7% and 6.4%.
- Fasting blood glucose in mg/dl: between 100 and 125
- 75-g-oGTT (oral glucose tolerance test) in mg/dl: between 140 and 199
Notice:
A one-time test result does not make you diabetic yet, but if you reach these levels more frequently, it stands to reason that you have early diabetes.
Pre-diabetes risk factors are:
- Gender (women 50% more often than men)
- Overweight (BMI1 > 25)
- Obesity (BMI1 > 31)
- Overeating
- Lack of movement
- Gestational diabetes
- Too little sleep
- Cholesterol levels are too high (especially if HDL—cholesterol2 is too low)
1 BMI stands for “Body Mass Index”, which provides information on whether the relationship between body weight and height matches.
2 HDL cholesterol (high-density lipoprotein) is good cholesterol because, unlike LDL cholesterol, it does not cause the hardening of the arteries. A mnemonic for good and bad cholesterol: LDL = Let lie; HDL = Have you love!
Type 1 – Diabetes
Type 1 diabetes – most commonly occurs in children, adolescents, and young adults under the age of thirty. Since diabetes type 1 in the past occurred mainly in children and adolescents, it was called “juvenile” diabetes. In exceptional cases, type 1 diabetes can also be diagnosed later in life, which is referred to as type 1 diabetes – LADA (Latent Autoimmune Diabetes in Adults). Both variants affect about 4% of all people who have diabetes.
Elevated blood glucose levels characterize type 1 diabetes due to insulin deficiency. It is an autoimmune disease in which the beta cells of the pancreas become the target of immune mediators, resulting in damage to the cells and, initially, inefficient insulin production. As the disease progresses, the beta cells stop producing insulin altogether. The resulting insulin deficiency leads to an undersupply of glucose (sugar) in the body’s cells. Since glucose is no longer transported from the blood into the cells, the blood becomes hyperglycemic.
To compensate for the energy deficit in the cells, the body tries to use the fat reserves. The resulting waste products can only be broken down with difficulty, which leads to over-acidification (metabolic acidosis) of the body. If diabetes remains untreated, damage occurs to the blood vessels, cells, and organs. In the worst case, diabetic coma or even death of the patient occurs.
Affected individuals must take insulin every day to keep their blood glucose levels healthy, which is why the disease is also known as insulin-dependent diabetes mellitus.
How do you make a type 1 diabetes diagnosis?
You ask yourself, which blood glucose values are decisive for the diagnosis of diabetes type 1? Diabetes is diagnosed when blood glucose exceeds the following limits.
- Long-term sugar HbA1c in %: > 6,5 %
- Fasting blood glucose in mg/dl: > 126
- 75-g-oGTT (oral glucose tolerance test) in mg/dl: > 200
For type 1 diabetes, in addition to exceeding the blood glucose limits, an antibody test against beta cells or insulin is also required. These antibodies can usually be detected in affected individuals months to years before the onset of diabetes mellitus.
Type 1 diabetes risk factors are:
- Type 1 diabetes in the family history
- Autoimmune diseases
- Damage to the pancreas
- Viral diseases
- Physical stress
Type 1 diabetes LADA or “Latent Autoimmune Diabetes in Adults” translates as “hidden immune diabetes in adults”. Since LADA does not appear until adulthood, it is often confused with type 2 diabetes. However, LADA can be detected and thus clearly diagnosed by an antibody test at the doctor’s office.
Type 2 – Diabetes
About 80 -90 percent of people diagnosed as diabetic have type 2 diabetes. It is caused either by the insensitivity of cells to insulin or by a lack of insulin. Insulin resistance (=insensitivity) is the leading cause of type 2 diabetes in the early stages, leading to insulin deficiency in later stages. In the beginning, the pancreas increases insulin production to do something about the resistance of the cells. This results in the pancreatic beta cells “burning out” due to excessive and continuous insulin production. Once this occurs, insulin deficiency begins, as insufficient or no insulin is produced.
But how should the interaction of hormones, cells, and blood sugar work? The hormone insulin is produced in the beta cells of the pancreas. When excess glucose is in the blood, the pancreas increases production, making more insulin available. The insulin acts as a door opener for the sugar in the blood to enter the cells, where the glucose is immediately used or stored as fats. The result is a falling blood sugar level; as soon as it falls below a certain level, the body produces the hormone glycogen in the pancreas. The release of the hormone is carried out by the alpha cells and reduces insulin production. The result is an optimal level of blood glucose.
Type 2 diabetes is exacerbated by obesity because insulin resistance is directly related to the body’s fat stores. Adult-onset diabetes mellitus and insulin resistance are the most common type 2 diabetes. “adult-onset diabetes” and “insulin-resistant diabetes” is also used to describe type 2.
It’s possible that your parents or grandparents referred to it as “having a little sugar.” Unfortunately, statistics show more and more that it is not due to age, because those affected are getting younger and younger.
How to diagnose diabetes type 2
You ask yourself, which blood glucose values are decisive for the diagnosis of type 2 diabetes?
- Long-term sugar HbA1c in %: > 6,5 %
- Fasting blood glucose in mg/dl: > 126
- 75-g-oGTT (oral glucose tolerance test) in mg/dl: > 200
Since type 2 diabetes usually occurs at an advanced age, from around 40 years onwards, it is typically sufficient to exceed the threshold values to make a diagnosis. In the early years, an antibody test against the beta cells or insulin should be carried out in any case for an exact diagnosis. This can determine with certainty whether the disease is not diabetes type 1.
Type 2 diabetes risk factors are:
- Pre-diabetic
- Type 2 diabetes in the family history
- Overweight
- Obesity with insulin resistance
- Disturbed lipid profile (low HDL, high LDL)
- Hypertension
- Africans, Asians, and Native Americans are at increased risk for
Type 3 – diabetes (other specific types of diabetes)
The term type 3 diabetes is used as a catch-all. It groups various rare forms of diabetes. The criterion for inclusion in this category is that diabetes develops differently from type 1 or type 2 diabetes. Type 3 diabetes comprises eight clinical pictures and the intermediate types of type 1 and 2 LADA. The abbreviation LADA stands for “Latent Autoimmune Diabetes in Adults”.
Type 3 diabetes includes the following subgroups:
- Diabetes Type 3a: MODY results from defective genes in the beta cells of the pancreas. Diabetes MODY (Maturity-Onset Diabetes of the Young) translates as “adult-onset diabetes in adolescents”, i.e., between birth and the age of 25. Currently, eleven subgroups with different symptoms are known.
- Type 3b diabetes: Caused by genetic defects in insulin action
- Diabetes type 3c: pancreopriver diabetes is caused by diseases of the pancreas
- Diabetes type 3d: is caused by disorders of the endocrine system. Among other things, diabetes insipidus should be mentioned here. In this case, there is a failure of osmoregulation of the body. This comes from the deficiency or lack of action of the hormone ADH. The result is exceptionally high urine excretion of up to 25 liters per day and the resulting overload of the kidneys.
- Diabetes type 3e: caused by chemicals or drugs. An example of this would be diabetes, which is steroid-induced: Steroids such as corticosteroids are the manufactured versions of hormones that raise blood sugar levels.
- Inflammation plays a variety of roles; examples would be severe asthma, arthritis, inflammatory bowel disease, and cystic fibrosis. Due to clinical benefits, steroid medications are used to reduce inflammation levels.
- Diabetes type 3f: caused by viruses
- Diabetes type 3g: caused by autoimmune diseases
- Diabetes type 3h: Caused by genetic syndromes
How to make a diabetes type 3 diagnosis
You ask yourself, which blood glucose values are decisive for the diagnosis of diabetes?
- Long-term sugar HbA1c in %: > 6,5 %
- Fasting blood glucose in mg/dl: > 126
- 75-g-oGTT (oral glucose tolerance test) in mg/dl: > 200
While diabetes type 1, type 2, and gestational diabetes are very well known, these particular types are also unknown to many doctors. Since there are countless variants of the disease, further testing and analysis are inevitable. A specialist can help, advise and guide you on your way.
Type 4 diabetes – gestational diabetes (gestational diabetes)
The bad news first, gestational diabetes usually does not cause typical symptoms, but it is one of the most common pregnancy complications. According to statistics from 2017, about 6% of all pregnancies in Germany are affected. Looking at the past 15 years, the number of expectant mothers affected by gestational diabetes has increased significantly. This is why all women are tested for diabetes in their pregnancy between the 24th and the 28th week.
How do you make a gestational diabetes diagnosis?
Gestational diabetes is present when any of the following values are reached on the 75-g-oGTT (oral glucose tolerance test):
- fasting: > 92 mg/dl (5.1 mmol/l)
- 1-hour: ≥ 180 mg/dl (10.0 mmol/l)
- 2-hour: > 153 mg/dl (8.5 mmol/l)
What are the gestational diabetes risk factors?
Women who carry twins or multiples have a higher risk of developing gestational diabetes. Whether you had one child or multiple births, the risk increases with each new pregnancy!
Other risk factors include:
- Pre-diabetic women or women with type 2 diabetes
- Your family history (do your parents, grandparents, or siblings suffer from diabetes?).
- Age over 25
- BMI greater than 30
- Gestational diabetes during a previous pregnancy
- Repeated miscarriages
- Birth weight of previous children over 4,500 grams
- Taking certain medications (antihypertensives, cortisone)
- Polycystic ovary syndrome
- Smoking
- Race (African, Asian, or Native American women are at higher risk for gestational diabetes).
- High blood pressure is a risk factor
- Polycystic ovary syndrome can cause gestational diabetes
The good news is that diabetes disappears after pregnancy, but this does not mean anything about the future risk of developing diabetes.
Causes of diabetes
Depending on the type of diabetes you suffer from, the cause of your elevated blood glucose level may be different. However, one fact is indisputable: insulin plays a role in every case. The result is always the same. Cells can no longer absorb the sugar from the blood.
The consequence; is significantly increased blood glucose levels up to hyperglycemia, which can lead to coma and even be fatal. It is important to note that you are not to blame for having diabetes mellitus. Diabetes is in your genes or usually linked to another disease. Your good or bad lifestyle is secondary but can be the decisive point.
In the following sections, we explain in detail the diabetes causes.
Pre-diabetes
For people in the pre-diabetes stage, the metabolic process and the associated transport of sugar from the blood into the cells no longer function properly. On the one hand, this results from your predisposition; on the other hand, your lifestyle and habits have a significant influence: unhealthy diet, too little exercise, and a stressful everyday life combined with too little sleep.
Type 1 – Diabetes
There are various causes of type 1 diabetes. It is almost always a disease of the immune system. The insulin-producing beta cells in your pancreas are attacked and destroyed by the body’s immune system. Why this happens is still unclear today.
Type 1 diabetes is inherited in most cases (but not always). If one parent, or even both, has diabetes, the probability for the child also increases.
Viral infections and other environmental factors may also play a role in the remaining cases.
Type 2 – Diabetes
Type 2 diabetes is caused by insulin resistance. This can be inherited, caused by an incorrect lifestyle, or also be due to advanced age.
In addition, certain intestinal hormones are not produced sufficiently in type 2 diabetes. These include, in particular, GLP-1 (glucagon-like peptide-1), which is made in the intestine and released into the blood when food is ingested. It regulates sugar metabolism by stimulating insulin production and inhibiting the production of glucagon (hormone and antagonist of insulin). GLP-1 also maintains the feeling of satiety and inhibits intestinal emptying. GLP-1 is broken down relatively quickly by the enzyme DPP-4 (dipeptidyl peptidase-4). The limited production and rapid degradation of GLP-1 results in a deficiency, which is the cause of impaired sugar utilization.
Not only hormones influence our sugar metabolism, but proteins such as SGLT-2 (sodium-glucosecontrasporter-2) in our kidneys. This protein is usually responsible for sugar recovery (reabsorption) from the urine. This makes sense in healthy people because sugar fuel is not lost as a valuable energy source for maintaining bodily functions. Ironically, this protein is increased in people with diabetes suffering from type 2. Thus, the kidney helps to maintain elevated blood sugar levels.
Type 3 – Diabetes
The diabetes type 3 group, in particular, is pervasive in this regard. Type 3 diabetes serves as a “catch-all” for unusual types of diabetes that genetic defects can cause, infections with viruses, medications, abuse of drugs and alcohol, metabolic disorders, or inflammation of the pancreas.
Type 4 diabetes- gestational diabetes (gestational diabetes)
What causes gestational diabetes cannot be answered today. It is suspected that pregnancy-related changes in hormone metabolism are the reason. It could also be due to increased calorie intake during pregnancy, more likely a combination of both.
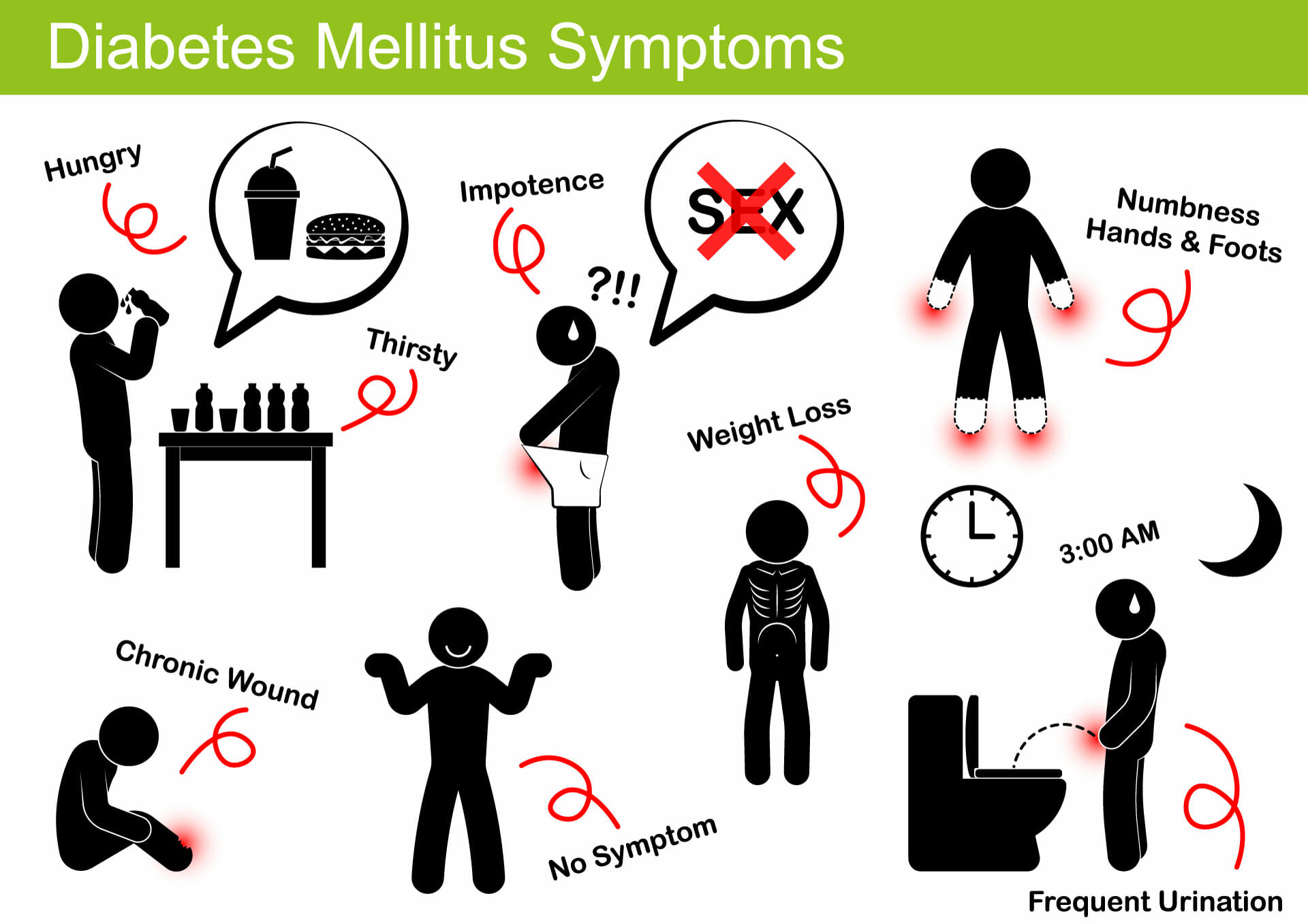
Diabetes symptoms
Diabetes mellitus is divided into different types based on the cause of its development and the resulting complications in the body.
Don’t just pay attention to symptoms. Find out about your family history early on. Are there diabetes cases in your family, parents, or grandparents?
Below we explain the most common diabetes symptoms.
Pre-diabetes
Pre-diabetes symptoms cannot be stated as precisely as for the other types. People with this pre-diabetes may show some of the known symptoms.
Pre-diabetes symptoms include:
- Hypoglycemia
- Constant thirst
- frequent urination
- increased fatigue
- Visual disturbances
- Acanthosis nigricans is a skin disease
Type 1 diabetes
Elevated blood glucose levels characterize type 1 diabetes due to insulin deficiency. These patients have no choice but to take insulin daily to stabilize their blood glucose levels. This is why the disease is also called insulin-dependent diabetes mellitus.
The symptoms vary depending on the blood glucose level and duration of diabetes, the symptoms vary. In the initial phase, it is asymptomatic and starts with some common symptoms, but unfortunately, they are very non-specific.
These include:
- increased thirst (polydipsia)
- frequent urination (polyurea)
- Fatigue
- Muscle weakness
- Dry skin
- unexplained weight loss
- blurred vision
- Wounds and ulcers that heal slowly
- Irritability
- frequent bacterial or viral infections (the result of a weakened immune system)
- other autoimmune diseases such as “Graves’ disease”.
If you have cases of diabetes in your family tree, especially with parents or grandparents, you should pay attention to the symptoms and have regular check-ups with your doctor. Blood sugar, long-term sugar, and antibody tests are important indicators. But be careful. There are two subgroups, type 1a, in which antibodies against insulin can be detected in the blood, sometimes even years before the onset of the disease. In type 1b, on the other hand, this antibody test is inconclusive.
Type 2 diabetes
Type 2 diabetes, unlike type 1, develops over months or even years. Since the symptoms are pretty ambiguous, affected individuals usually learn of the diagnosis by chance. Only acute symptoms can harden the suspicion of diabetes type 2; these include:
- Intense thirst and the resulting urge to urinate:
- Both strongly condition each other. One leads to the other. This is triggered by the kidneys, which try to excrete the excess sugar through the urine. The intake of fluid compensates for the resulting loss of fluid.
- Fatigue, lack of concentration, and performance are caused by the lack of sugar in the cells.
- Weakened immune system and susceptibility to infections
- Dry skin and constant itching
- Weight loss
- Visual disturbances
- Poor wound healing
Type 3 diabetes
In general, the same symptoms occur in the diabetes type 3 family as in diabetes type 1 and diabetes type 2. However, the symptoms of the respective subgroup, i.e., the underlying disease, are also present.
Type 4 diabetes – gestational diabetes (gestational diabetes)
Gestational diabetes is usually asymptomatic and is diagnosed during screening tests in the second or third trimester of pregnancy. The early stages begin with some common symptoms that may vary from case to case. Common symptoms of gestational diabetes include:
- – Increased thirst (polydipsia)
- – Frequent urination (polyurea)
- – Increased appetite
- – Fatigue
- – Blurred vision in later stages
- – Irritability
- – Snore
The following typical symptoms are attributed to pregnancy:
- Increased blood pressure
- An increased amount of amniotic fluid
- Increased sugar content in urine
- Increased susceptibility to bladder infections
- Substantial increase in weight and size of the unborn child
One of the combinations of these symptoms is not enough to diagnose gestational diabetes, and it needs an appropriate blood glucose test.
Treatment and therapy of diabetes
The primary goal of diabetic care is to normalize blood glucose levels as much as possible. Controlling blood pressure and cholesterol levels is essential to diabetes management, as diabetes can increase the risk of heart disease and peripheral artery disease (better BKut vessels?).
People with diabetes are expected to manage their condition daily. Blood glucose levels, diet, exercise, weight control, and stress management are all part of this process. Based on this data, it quickly becomes apparent whether insulin administration is necessary.
Understanding how nutrition works, digestion occurs, and where the sugar in the blood comes from is essential.
Breaking down the foods you eat into numerous nutrients is part of the digestive process. When you eat carbohydrates, your body breaks them down into sugar/glucose (e.g., bread, rice, pasta)-which tends to go directly to KH. For glucose to reach its final destination, the body’s cells (tissues and organs are made up of cells), a “key” is required. Insulin is this “key” or “helper”. The hormone insulin is produced by the pancreas, an organ below the stomach, from where it enters the bloodstream and ensures that sugar is absorbed into the cells.
If you have diabetes,
- your pancreas either does not produce enough or has no insulin.
- Or your pancreas produces insulin, but your cells don’t respond to it, so your body can’t use it properly.
Both cause glucose not to enter the body cells; as a result, the blood glucose level rises.
To maintain the tools for self-control, there are two critical issues for people with diabetes and their families to address from the beginning.
- Take part in diabetes training.
- Keep a diabetes diary.
Pre-diabetes
Studies indicate that the most effective remedy for pre-diabetes is a lifestyle change. We refer to this as prevention, to avoid developing diabetes first, or to ease its possible progression. Changing habits, primarily in diet, exercise, and stress management, reduce the risk of developing diabetes by 40 to 70%.
- Lose weight
- Exercise (about 4 hours a week)
- Nutrition plan
Type 1 diabetes
Insulin-dependent diabetes mellitus is a name for type 1. Due to today’s medicine and proven treatment methods, life expectancy and quality of life are very high.
Since there is an absolute shortage of the hormone insulin, the person with diabetes has no choice but to supply insulin daily to regulate blood sugar. This can be done in different ways, for example, with a pen, a syringe, or an insulin pump.
When you ask your doctor about insulin, they will most likely mention three things:
- “WEAK ENTRY” refers to the time it takes for the medication to reach your bloodstream and begin working as insulin.
- “EFFECTIVE MAXIMUM” refers to the time it takes for insulin to get its maximum concentration in the blood.
- “EFFECTIVE DURATION” refers to the length of time that insulin is detectable in the blood and can exert its effects.
Insulin comes in different profiles of action
| Insulin type | Onset of action | Maximum effect | Duration of action |
| Very fast and quick | 5-20 min | 20-30 min. | 3 to 5 hrs. |
| Short effective | 30-60 min. | 2-4 hrs. | 5-8 hrs. |
| Intermediary | 1-2 hrs. | 4-6 hrs. | up to 18 h |
| long-acting | 1-4 hrs. | Not delimitable | Up to 24 (42) hrs. |
The amount of insulin needed depends on the following factors:
- Nutrition
- physical activity
- existing disease (among other infectious diseases)
- the presence of pregnancy
- Operations
- Stress level
You may be prescribed two insulin injections per day at the beginning of treatment. You may need more injections in the future.
Basis-Bolus-Concept is a proven form of therapy today. In this therapy, “BASAL insulin” is injected into the subcutaneous fatty tissue daily. From there, it is slowly broken down, i.e., it enters the bloodstream slowly and regularly. This ensures a constant primary supply. Bolus insulin is the administration of short-acting insulin before meals to reduce higher blood glucose levels.
To supply the right amount of insulin, it is necessary to know the blood glucose level. For this, it is indispensable to carry out a measurement. Here again, there are some possibilities nowadays, but the glucometer is best known. A drop of blood is put on a test strip, and after a short time, the result is known. With this result, you can calculate the exact amount of insulin with this value.
Type 2 diabetes
Type 2 diabetes can now be treated well but not cured. In discussion with your doctor, you should plan the goals of the treatment. Here, personal goals are agreed upon; for example, we could take the long-term sugar (HbA1c). Your goal would be to keep this value between 6.5 and 8.5%, depending on your age and state of health. Do not forget to formulate your plans S.M.A.R.T. and work towards achieving them.
There are several treatment options, ranging from diabetes education to exercise and a trained trainer to medication. One will probably start with metformin or a combination of other drugs. Your doctor will likely add other medications if this does not change the blood sugar.
The diabetes type two (but 5 points????) therapy measures at a glance:
- Slimming
- Change diet
- Movement
- Medication
- Insulin
(Does not fit the 1st paragraph regarding DM2)> Many people talk about diabetes type 2 being curable. This is correct if you look at the symptoms and the late effects. It is possible to become symptom-free/cured by the changes mentioned above in habits: To remain so, you must maintain them throughout your life.
Type 3 diabetes
Type 3 diabetes is a multi-faceted issue due to the myriad variations/causes. Given this, treatment is a very individualized issue, tailored to the exact subtype of the disease. Therefore, the particular steps, medications, and lifestyle changes depending on the specific cause.
The basis here is the exact diagnosis of which subcategory it is. The level of residual insulin production and how well the cells respond to it should also be determined.
Accordingly, the therapy is based on two pillars:
- Treatment of the respective underlying disease
- Treatment of diabetes, the goal is to get the blood glucose level to a stable level and maintain it.
In addition to constant monitoring of blood glucose, it is usually necessary to administer insulin. In addition, the diet should be adapted to the underlying disease. – The following generally applies
Type 4 diabetes – gestational diabetes (gestational diabetes)
It may already be enough to change a few of your habits in terms of diet and exercise. Pay attention to reducing carbohydrates, but beware, it is not a classic diet. It is usually not about losing weight by cutting down on carbohydrates but about redistributing carbohydrates to other energy sources such as protein or healthy fats.
Since insulin resistance is highest in the morning, blood glucose levels are usually higher than the rest of the day.
Here are a few tips on what to look for in a healthy diet:
- A low-carb breakfast might look like this:
- Dairy products such as yogurt or cottage cheese with fruit
- Eggs (omelet, scrambled, boiled egg, …)
- if cereals, then, e.g., wholemeal bread with cheese, salmon, ham
- Midwives recommend eating several small meals instead of fewer large ones (4-5 smaller meals daily).
- Otherwise, distribute the calorie portion evenly among the meals.
- Eat lots of vegetables, fiber, and fruit (which contains fructose!) only in moderation! We recommend 3-4 parts vegetables and 1-2 parts fruit.
- Avoid smoothies unless you make them yourself (recommendation. 4 parts vegetables and 1 part fruit).
If you take this to heart and regularly enjoy the fresh air with your loved ones during a long walk, in most cases, you will get through your pregnancy well despite and with your gestational diabetes.
You do it not only for you alone but also for your child!

In rare cases, it may be necessary to take insulin until the end of your pregnancy, since insulin action is increased in expectant mothers in the third trimester. You should take special care. This could lead to hypoglycemia (low blood sugar) if you supply the same amount. Therefore, blood glucose measurement and insulin administration should always be in close consultation with your gynecologist.
The procedure for gestational diabetes depends on the severity and should, in any case, be discussed and accompanied by a diabetologically trained physician. Depending on the original weight or the weight gain during pregnancy, it may be necessary to follow a specific diet.
After the birth of the child, another sugar test is automatically arranged. This is done to ensure you do not continue to suffer from gestational diabetes.
Six important pillars for successful diabetes therapy
Healthy diet
Often we have discussed it, and it is one of the main topics in the therapy and prevention of all diabetes diseases. But what does it look like?
- Beverages Water
- and unsweetened fruit or herbal tea (unlimited), 2-3 cups of coffee, and light or zero soft drinks are considered suitable.
- Unsuitable, on the other hand, are soft drinks with sugar, energy drinks, fruit juices, and alcohol.
- Important: Drink at least 1.5 to 2 liters a day
- Vegetables and fruits
- Eat at least three servings of fiber-rich, if possible, green vegetables and no more than two servings of fruit. One serving is equal to a handful. (total of 5 servings a day)
- Milk and dairy products
- about three servings a day. Make sure you do not overeat protein, protein because what is too much, the body converts into sugar.
- Meat and sausages
- 2-3 servings a week. Pay attention to the quality of the flesh. (1 portion =150-200g of beef or 30g of sausage).
- Fish2-3
- servings should be considered per week, preferably sea fish such as salmon, mackerel, etc. (1 serving = 150-200g fish)
- Sweets and fast food
- You
- should give up entirely, but it is difficult because of the quality of life.
- If, then you should only resort to fast food once a month. For sweets, there are lovely low-sugar alternatives. But please, no more than a tiny serving a day.
Here are a few examples of a healthy diet that is low in carbohydrates. These are from our cookbook, either follow the links or filter by your requirements under cooking and recipes. Bon appetite and have fun cooking them up.
Exercise and sport
No one expects you to become a competitive athlete and do 15 hours of sports a week. After all, going from 0 to 100 would be far too dangerous in terms of form. But what does the right start look like?
- More movement in everyday life
- It is better to take the stairs than the elevator or escalator
- Get off the train one stop before and walk the rest of the way
- To work by bike
- Use a pedometer for control and motivation
- More intensive exercise (3 × 30 minutes a week in the beginning)
- Walking
- Jogging
- Bicycle ride
- Swimming
- Hiking
- Strength training
Self-control
Keep a diabetes diary and note down the results of your blood glucose measurements, the food you ate, what and how much you drank, and your exercise or workout. Also, note how they felt and how they were doing.
Weight loss
If you stick to the first three points, you usually do not need to diet to lose weight. As a rule, your previous life was characterized by wrong food and inactivity. You have changed this in the meantime.
Tablets / Insulin
If necessary, medication and constant monitoring also play an essential role. Insulin, in particular, must be adjusted to the daily requirement.
Regular training
Training courses are a fundamental part of diabetes treatment. They teach you everything you need to know about diabetes and give you the tools to make your treatment successful. Training is provided by various institutions and also by your health insurance company.
Diabetes emergency: simply react correctly!
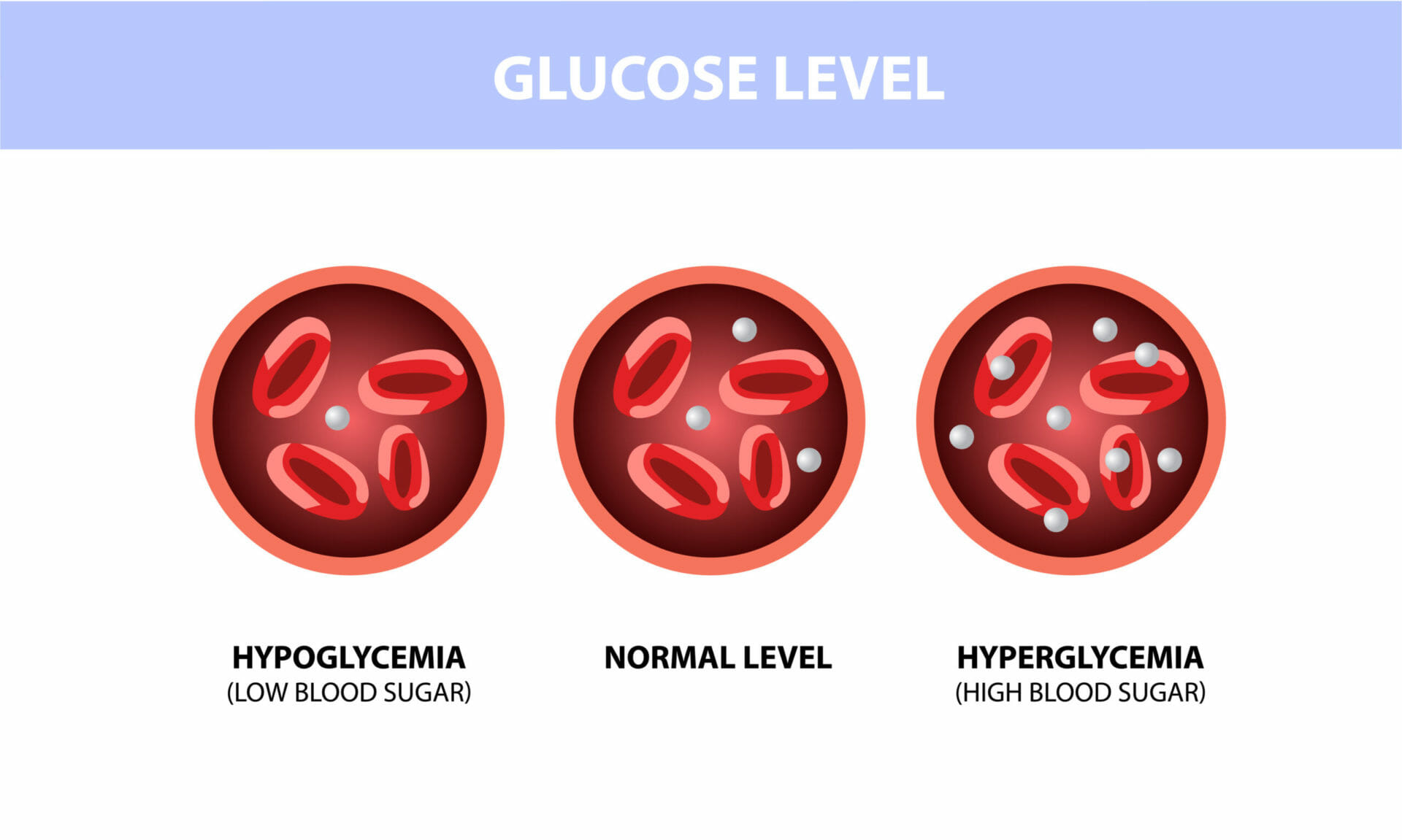
Acute hypoglycemia or hyperglycemia is an emergency for people with diabetes. The extent to which they occur depends on a diabetic’s metabolism and how well they are controlled. In both cases, a response is needed, and haste is required.
Hypoglycemia (low blood sugar)
Hypoglycemia or “hypo” stands for hypoglycemia of the body – the limit value is 50 mg/dl. If the blood glucose level is lower than this, it is called hypoglycemia. Any person with diabetes who takes insulin in any form can suffer from hypoglycemia.
Causes of hypoglycemia may include:
- Insulin or oral antidiabetic drug overdose
- Too little energy supply
- Excessive energy consumption due to heavy physical strain
- Alcohol consumption
- Vomiting or diarrhea
- too big a splash-eat distance
Symptoms of hypoglycemia:
- Sweating
- Trembling
- Palpitations
- Nervousness
- Headache
- Craving
- Dizziness
- Concentration and visual disturbances
- Disorders of fine motor skills
If blood glucose levels continue to drop, hypoglycemic shock may occur. Disorientation, paralysis, seizures, and unconsciousness may occur. All these conditions constitute an acute emergency.
Immediate measures in case of mild hypoglycemia (40-60 mg/dl)
- Intake of 20 g of carbohydrates.
- If there is no improvement after 15 minutes and the blood glucose has not risen to a level above 50-60 mg/dl, repeat the intake of 20 g of carbohydrates.
- You ensure that the blood sugar stabilizes with a (small) meal (fruit, wholemeal bread, yogurt).
What corresponds to 20g of carbohydrates? 4 bars of dextrose, or 200ml of soft drinks (not light or zero) or fruit juice. NO sugar-free drinks or foods!
Immediate action in case of severe hypoglycemia (< 40 mg/dl)
The person is still conscious but shows extreme signs of hypoglycemia. The person is no longer able to help themselves.
- Intake of 30 g of carbohydrates
- If there is no improvement after 15 minutes and the blood glucose has not risen to a level above 50-60 mg/dl, repeat the intake of 30 g of carbohydrates.
- You ensure that the blood sugar stabilizes with a (small) meal (fruit, wholemeal bread, yogurt).
What corresponds to 30g of carbohydrates? 6 bars of dextrose, or 300ml of soft drinks (not light or zero) or fruit juice. NO sugar-free drinks or foods!
Immediate measures in case of severe hypoglycemia (< 40 mg/dl) with unconsciousness
- Inform emergency physician
- Stable lateral position
- Do not instill drinks or similar because of the risk of choking
- Clean mouth from food debris and remove loose dentures.
- Glucagon injections (subcutaneous or intramuscular in the thigh)
- Immediate help with glucose after waking up
No matter how severe the hypoglycemia is, you should always discuss it with your doctor. Work out with him how it could have happened and how you can avoid hypoglycemia in the future.
There are also cases in which patients do not notice the symptoms of hypoglycemia and thus cannot react in time. In older people, circulatory disorders in the brain and their signs are mistaken for hypoglycemia; here, caution is advised.
Hyperglycemia (ketoacidosis)
Metabolic acidosis of the blood and body are acute complications that can occur with elevated blood glucose. Here we distinguish two forms.
Diabetic ketoacidosis occurs predominantly in type 1 diabetes
Blood glucose levels above 250 mg/dl indicate diabetic ketoacidosis and are usually caused by infections. The body lacks insulin. Therefore, the cells are not supplied with sufficient sugar. Thus, the body starts to compensate for the deficit with fat and produces ketones for this purpose. This process leads to acidification of the body.
Symptoms of ketoacidosis:
- Increased urination and a strong feeling of thirst
- Loss of appetite, nausea, and vomiting
- Abdominal pain
- Acetone odor in the breath (smell like nail polish remover or mouse urine)
- Deepened breathing
- tiredness, drowsiness, a feeling of weakness
- Weight loss
Hyperosmolar dehydration syndrome occurs predominantly in type 2 diabetes
Hyperosmolar dehydration syndrome occurs when you have consumed too little fluid over a long period. This builds up over several days or even weeks. Infections and errors in insulin therapy cause blood glucose levels to rise above 600 ml/dl. As a result, there is a significant loss of fluid, equivalent to dry the body.
Symptoms of hyperosmolar dehydration syndrome:
- Fatigue
- frequent urination, increased thirst
- blurred vision
- Calf cramps
- Weight loss
- Low blood pressure
- Dizziness, speech disorders, dysphagia
Immediate action for blood glucose levels above 250 mg/dl and elevated ketone levels (urine test strips 2+/3+):
- Notification of a doctor/emergency physician
- In case of vomiting, immediate admission to hospital
- Inject insulin
- drink very much
- Avoiding physical exertion
- not fall asleep
Regardless of which of the two cases it is, the doctor should decide what further treatment looks like. If the case is relatively mild, outpatient therapy could be opted for; in severe cases, the affected person should be treated in a hospital in any case. Both forms can lead to diabetic or hyperosmolar coma if left untreated.
Health consequences of diabetes (secondary diseases)
Diabetes is a significant problem for a person’s overall health and well-being as it increases the risk of certain diseases such as high blood pressure, cardiovascular issues, and even malignancies. Individuals with a BMI over 40 are more susceptible to the health problems caused by diabetes, which can include insulin resistance, high blood pressure, and cardiovascular disease.
Some health conditions associated with diabetes are:
- Cardiovascular diseases: These include high blood pressure, high blood cholesterol, arteriosclerosis leading to arterial occlusions and strokes, coronary artery disease, angina pectoris, and heart attacks.
- Diabetic neuropathy,
- Kidney problems: Diabetic nephropathy, which can lead to kidney failure.
- Eye diseases: Diabetic retinopathy can cause blurred vision or even blindness
- Foot ulcers, are caused by nerve damage and can be difficult to heal
- Erectile dysfunction / potency disorder
- Skin infections
- Impairment of hearing
- Dementia in elderly patients due to developing nerve damage in the brain.
Pre-diabetes
Pre-diabetes is talked about less regarding health consequences and more as a risk factor for diabetes and cardiovascular disease. Studies have shown a close link between pre-diabetes and obesity, altered blood lipid levels, low HDL cholesterol, and high blood pressure.
Type 1 diabetes
Blood glucose levels and, consequently, hemoglobin A1c, are permanently elevated. This is referred to as hyperglycemia. This high glucose level damages the small and large blood vessels and nerves. Possible consequences are:
- Diabetic neuropathy causes tingling & nerve pain
- Diabetic nephropathy leading to kidney failure
- Diabetic retinopathy can affect vision
- Cardiovascular diseases
- Hypertension
- Increased risk of stroke
- Diabetic foot(Explanation? Symptoms?
Type 2 diabetes
Type 2 diabetes causes many problems that depend on the person’s age, the duration of diabetes, and the control of blood glucose levels. Patients with poorly controlled diabetes are more susceptible to developing health consequences, which may include:
- Hypertension
- Stroke
- Blindness
- Kidney failure
- Higher susceptibility to foot infections and ulcers
- Nerve damage leading to neuropathy
- Hearing loss
- Alzheimer’s disease
Type 3 diabetes
The health consequences are the same in diabetes type 1 and type 2. Since in diabetes type 3, the many late complications meet different clinical pictures, this complicates the primary disease. These acute and chronic complications determine, among other things, the patient’s life expectancy with type 3 diabetes.
Type 4 diabetes – gestational diabetes (gestational diabetes)
Gestational diabetes can affect the health of both the mother and the fetus. Some of the health complications caused by gestational diabetes may include:
- Premature birth (Preterm):
Gestational diabetes increases the risk of premature birth. This is because high blood glucose levels in the mother can lead to early labor and delivery of the baby before the end of pregnancy. Premature babies are more susceptible to breathing problems and infections.
- Excessive birth weight:
Suppose blood glucose levels are higher than usual during pregnancy. In that case, the baby’s birth weight may increase, making it difficult for the baby to emerge from the birth canal during delivery and more susceptible to birth injuries. A cesarean section is required to deliver such large babies from diabetic mothers.
- Severe respiratory distress:
Early birth can put the baby in severe birth difficulties due to immature lungs. Respiratory distress syndrome is due to the lack of surfactant in the alveoli, which makes breathing difficult. Therefore, these babies are more prone to brain damage due to the poor oxygen supply in premature births.
- Low blood sugar level (hypoglycemia):
Early after birth, the newborn can enter severe hypoglycemia, which leads to seizures and brain damage due to poor glucose and the metabolic function of neurons.
- Obesity and type 2 diabetes later in life:
Babies born to mothers with gestational diabetes have a higher risk of becoming obese and developing type 2 diabetes mellitus later in life.
- Stillborn:
If gestational diabetes remains undiagnosed or untreated, it can lead to fetal death before, during, or immediately after birth. Therefore, early diagnosis by blood glucose measurement between 24 and 28 weeks of gestation is recommended to avoid further complications.
- Preeclampsia:
Preeclampsia is a condition characterized by high blood pressure during pregnancy. Gestational diabetes can increase the risk of preeclampsia, leading to difficulties during pregnancy, such as heavier bleeding during a C-section. These complications can endanger the life of the mother and the baby.
- Cesarean section:
Gestational diabetes can lead to complications, such as a larger, overweight fetus that is difficult to deliver through expected vaginal delivery (NVD). Therefore, a cesarean section must be performed to have the baby.
- Future diabetes in the mother:
Women with gestational diabetes are at increased risk of developing type 2 diabetes later in life due to insulin resistance.
Prevention
Pre-diabetes
Several international studies show that early lifestyle changes and medication significantly reduce the risk of developing diabetes. The studies show that the risk of the onset of diabetes can be prevented or delayed in almost 60% of those affected by lifestyle changes. With early drug treatment, the rate is about a quarter of those involved. In the Finnish “Diabetes Prevention Study (DPS)”, in which subjects with impaired glucose tolerance were followed for three years, it was found that the rate of disease could be reduced from 22.9 % to 10.2 %. This corresponds to a 58 % diabetes risk reduction, achieved by adjusting eating habits, exercise, and stress management.
Diabetes type 1
Type 1 diabetes can be effectively controlled/positively influenced by regular exercise. However, improving your health by jogging is not as simple as that. Regular physical activity affects blood glucose levels. Therefore, routine housework or gardening must be carefully coordinated with insulin dosing and food intake. The more you know, the better. Be sure to monitor your blood sugar levels during an exercise session to see how/the activity affects you and your sugar. Specific activities may raise your blood sugar levels, while others may not. If your insulin level is too low, you can lower it or have a high-carbohydrate snack. The motto is, better to check once too often!
You should check your urine for ketones if your blood sugar is above 240 mg/dL. Ketones are formed when blood sugar is too high and over-acidifies your body. If the urine is unremarkable, everything is fine, and you can continue with peace of mind. If the value is too high, simply skip the workout and do something for your soul.
It’s also important to understand how foods affect your blood sugar. Knowing the role carbohydrates, fat, and protein play will help create a healthy eating plan. Seek advice from a diabetes educator or qualified dietitian. To get started, you can also find nutrition plans to get you through the first few weeks.
As you can see, you can positively influence type 1 diabetes with minor adjustments to your lifestyle, ideally to the extent that you can reduce your daily insulin. But please always do this in consultation with your doctor.
Diabetes type 2
As already described in pre-diabetes prevention, early diagnosis, a change in habits, and, if necessary, appropriate medication is a promising way of diabetes prevention.
You should change your eating habits, healthy fresh food, lots of vegetables and fruits (4 parts vegetables and 1 part fruit), and food with complex carbohydrates like whole grains, which are also high in fiber. These keep your blood sugar stable and, at the same time, are essential for your intestinal health.
Exercise and sport are also on the agenda, but watch your blood sugar and ketone levels here too.
Type 3 diabetes
Prevention of type 3 diabetes is more complicated than in the other variants. There are many different causes, and not all underlying diseases can be prevented.
The best prevention mentioned here is a healthy lifestyle, no alcohol or drugs, a balanced and healthy diet, sufficient exercise, and the renunciation of nicotine.
Type 4 diabetes – gestational diabetes (gestational diabetes)
Gestational diabetes can be prevented by adopting healthy habits before pregnancy. Early diagnosis and prompt treatment in consultation with your doctor are also necessary; however, these vital steps can reduce the likelihood of gestational diabetes. If you had gestational diabetes in the previous pregnancy, you are more likely to develop diabetes during and after pregnancy than an average woman. Gestational diabetes can be managed through healthy lifestyle changes, such as quitting smoking and alcohol, controlling your eating and sleeping habits, and stress management. Some health-promoting measures are necessary to prevent gestational diabetes and its complications.
- Eat healthily: Gestational diabetes can be prevented through healthy eating habits. Consume foods rich in fiber and nutrients, such as vegetables, fruits, and grains. Avoid foods high in carbohydrates and fats. Keep control of your daily calorie consumption.
- Stay active: gestational diabetes can be prevented by regular exercise. Avoiding a sedentary lifestyle before and during pregnancy is vital for maintaining a healthy weight. Light to moderate physical activity of at least 30 minutes daily can reduce the risk of gestational diabetes. A short walk in the morning benefits the mother’s health as it reduces stress, improves mood, and helps her stay active.
- Start pregnancy at a healthy weight: If you plan to get pregnant, keep your weight within the recommended limits. Women with a BMI greater than 30 are more prone to gestational diabetes. Losing weight before pregnancy can help keep it off. Watch your eating habits and exercise regularly to maintain a healthy weight and ensure a safe pregnancy.
- Seek regular medical advice: Regular medical examinations and blood glucose measurements can help prevent complications of diabetes mellitus.
- Monitor your blood glucose levels: It is essential to monitor your blood glucose levels during pregnancy. About 2-10% of women are diagnosed with gestational diabetes during pregnancy. Undiagnosed cases can lead to severe complications during delivery. Therefore, it is vital to take all precautions before and during pregnancy.
Is diabetes curable?
Is prediabetes curable?
Pre-diabetes is the precursor to type 2 diabetes. It is defined by blood glucose levels above average but still below the threshold of diabetes. Therefore, nothing is lost yet. With the appropriate treatment, changing one’s habits and the associated healthy diet, sufficient exercise, and active stress management, pre-diabetes can be cured – or the levels can be returned to the normal range.
Is type 1 diabetes curable?
Type 1 diabetes is currently not curable, as the insulin production in the pancreas or the metabolism is irreparably damaged. An affected person can lead a largely symptom-free life thanks to modern therapy methods.
Is diabetes type 2 curable?
The bad news first, type 2 diabetes is not curable! But if you have changed your life, you have a good chance to live symptom-free. The motto is “You have to change your life” – diet, exercise, and stress must be brought to normal levels. Losing weight is the watchword; according to one study, an average of 15 kg. This way, the disease can be “cured” because of the second half of the motto; “You have to live your change!” As long as you follow the advice and healthy habits, you will likely have a long life ahead of you without signs of diabetes.
Type-3 diabetes curable?
Yes and No. There are many underlying diseases, making the diagnosis of type 3 diabetes difficult. Often this form of diabetes is confused with type 1 or type 2. In some cases, just taking an antidiabetic drug would be enough.
As with all other forms, it is crucial to jettison one’s bad habits and steer one’s lifestyle in a healthy, sustainable direction. A healthy diet, exercise, and stress management are essential. One more tip about nutrition, some forms make a specific diet necessary to support the treatment of the underlying disease.
Type-4 diabetes – gestational diabetes curable?
Gestational diabetes usually “cures” itself shortly after the placenta is expelled. After 5-10 years without symptoms, diabetes type 2 develops in 25-50% of all mothers.
References:
- http://www.diabetes-wiki.org/
- https://pflegebox.de/ratgeber/krankheiten/diabetes
- https://www.patienten-information.de/kurzinformationen/diabetes-therapie
- Diabetes mellitus Typ 3 – DocCheck Flexikon Prävention des Diabetes mellitus Typ 2 — Deutsch (uniklinikum-dresden.de)
- Auswirkungen von Typ-1-Diabetes » Typ-1-Diabetes » Krankheiten » Internisten im Netz » (internisten-im-netz.de)
- Schwangerschaftsdiabetes: Ursachen, Risiken, Behandlung – NetDoktor
- https://www.docsonnet.com/de/diabetes
- https://www.diabetesschweiz.ch/
- https://www.zuckerkrank.de/